Written by: Dr. Claire Arcidiacono, ND
For further questions or concerns email me at carcidiacono@invitehealth.com†

In our last blog we discussed dementia. Today we will be talking about Alzheimer’s disease. As I stated last time Alzheimer’s disease (AD) is one of the many causes of dementia. In this blog we will review what is Alzheimer’s disease? Exactly how does it affect the brain? Be prepared to refer to my blog on anatomy if you need to. Since this is such an important topic, I WILL be breaking it down into two parts with the next blog concentrating on known risk factor for developing Alzheimer’s as well as how is it diagnosed and what you can do to mitigate the risks. Lastly in our next blog we will review what you can do to help with symptom management. †
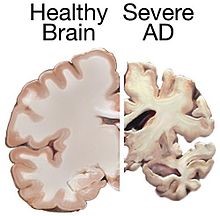
Alzheimer’s disease is a neurodegenerative disease. (1) What this literally means is that there is both structural and functional damage to the neurons. This neuron damage eventually leads to the neuron or cell death. This leads to structural changes we can actually see in the brain. (2) Please see the attached picture! (3)
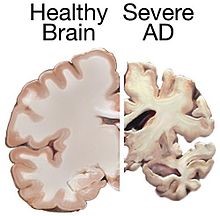
Now if you want to bring up the anatomy blog now would be a great time! If you remember it that is fantastic! Well as I said then, the information presented there would be relevant now. Alzheimer’s as I’ve stated leads to the loss of neurons. This occurs in the cerebral cortex. It also occurs in the temporal lobe, the parietal lobe and the frontal cortex. AD affects each of these parts of the brain and thus has symptoms that occur due to the dysfunction of these parts of the brain. (4) I know you might be thinking what about the amyloid plaque? Isn’t that something I’ve heard of that is related to how AD affects the brain? This is an important topic however since its presence is more of a risk factor for developing the disease, I’ll talk about it more when I get into those details. †
BRAIN HEALTH & MEMORY, PART 2: BRAIN ANATOMY>>READ NOW!
Everyone knows that AD affects memory. The signs and symptoms of the disease typically worsen as the disease progresses; hence it is broken into 3 stages. These are the early/mild, moderate and late/severe stages. The disease starts by affecting the short-term memory. In practicality this means that there is trouble remembering things you just learned or even just trouble in recalling new information. As the disease progresses long term memory begins to become affected as well. Early signs of the disease can also include problems with activities of daily living. These can include problems with attention, planning, flexibility and abstract thinking. Having difficulty with semantic memory can also start to occur. In these first or early stage, there is the beginning of apathy and depression. (5) While in most people with AD the early-stage memory changes and difficulty learning is what leads you to going to the doctor for help and eventually a “diagnosis” in a small percentage where there are other more prominent symptoms. These include language difficulties and problems with executive functions, perception and execution of movement. (6) The way that AD affect language includes a decrease in vocabulary as well as a decrease in word fluency. While certain movement coordination and planning difficulties may be present, they are usually not severe at this stage. (5) As I’ve previously mentioned in the early-stage, short-term memory is affected first with older memories and implicit memory (this is the body’s memory of how to do things such as use a fork) are not affected until the disease progresses. † (7)
As the disease progresses to moderate, the symptoms become more severe. For example, speech becomes more difficult due to the problems with vocabulary. Reading as well as writing skills also deteriorate as the disease progresses. Due to the decrease in coordination, the risk of falling also increases over time. It is during this stage that long term memory begins to become impaired. It is at this time that the individuals may fail to recognize close relatives. Behavioral and psychiatric changes also start to occur at this stage. These include wandering, irritability, emotional lability and aggression. (8) AD is associated with a phenomenon known as sun-downing, which is basically where symptoms become worse as the natural sunlight begins to decline. (9). Approximately 30% of people with AD experience delusional symptoms. Lastly in this stage, incontinence can start to develop. † (9)
The last stage is also known as the final stage. In this stage an individual can no longer perform activities of daily living and thus must rely on a care giver. Language is reduced to very simple phrases or even simple words. In time verbal language is entirely lost. Although aggression may still occur more commonly, apathy is seen at this stage. At this point muscles have deteriorated to the point where an individual is bed ridden and unable to feed themselves. Usually, death occurs due to an outside source such as bed sores. † (10)
In summary, in those that are over 65 or have a family history of Alzheimer’s disease it is important to watch out for any changes in memory, behavior, mood and even their ability to communicate. If you notice any changes or “just don’t feel right” it is important to get help. †
DEMENTIA, INVITE HEALTH BLOG>>READ NOW!
In our next blog we review risk factors/ tests as well as any natural treatments that have been studied and found to help with mitigating these risks and the symptoms of Alzheimer’s. †
REFERENCES
- “Dementia Fact sheet”. World Health Organization. September 2020.
- Pereira, TMC; Côco, LZ; Ton, AMM; Meyrelles, SS; Campos-Toimil, M; Campagnaro, BP; Vasquez, EC (20 November 2021). “The Emerging Scenario of the Gut-Brain Axis: The Therapeutic Actions of the New Actor Kefir against Neurodegenerative Diseases”. Antioxidants. 10 (11): 1845. doi:3390/antiox10111845. PMC 8614795. PMID 34829716.
- https://en.wikipedia.org/wiki/Neurodegenerative_disease#/media/File:Alzheimers_brain.jpg
- Wenk GL (2003). “Neuropathologic changes in Alzheimer’s disease”. The Journal of Clinical Psychiatry. 64 Suppl 9: 7–10. PMID 12934968.
- Bäckman L, Jones S, Berger AK, Laukka EJ, Small BJ (September 2004). “Multiple cognitive deficits during the transition to Alzheimer’s disease”. Journal of Internal Medicine. 256 (3): 195–204. doi:1111/j.1365-2796.2004.01386.x. PMID 15324363. S2CID 37005854.
- Förstl H, Kurz A (1999). “Clinical features of Alzheimer’s disease”. European Archives of Psychiatry and Clinical Neuroscience. 249 (6): 288–290. doi:1007/s004060050101. PMID 10653284. S2CID 26142779.
- Carlesimo GA, Oscar-Berman M (June 1992). “Memory deficits in Alzheimer’s patients: a comprehensive review”. Neuropsychology Review. 3 (2): 119–169. doi:1007/BF01108841. PMID 1300219. S2CID 19548915.
- Carlesimo GA, Oscar-Berman M (June 1992). “Memory deficits in Alzheimer’s patients: a comprehensive review”. Neuropsychology Review. 3(2): 119–169. doi:1007/BF01108841. PMID 1300219. S2CID 19548915.
- Volicer L, Harper DG, Manning BC, Goldstein R, Satlin A (May 2001). “Sundowning and circadian rhythms in Alzheimer’s disease”. The American Journal of Psychiatry. 158 (5): 704–711. doi:1176/appi.ajp.158.5.704. PMID 11329390. S2CID 10492607.
- Frank EM (September 1994). “Effect of Alzheimer’s disease on communication function”. Journal of the South Carolina Medical Association. 90 (9): 417–423. PMID 7967534.