Digestive Health Part 8: Diverticulosis Vs Diverticulitis

Written by Dr. Claire Arcidiacono, ND diverticulosis
For further questions or concerns email me at [email protected]†
Last week we talked about Irritable Bowel Disease and Irritable Bowel Syndrome. Today we’ll be covering the difference between Diverticulosis and Diverticulitis, which involves the formation of small, bulging pouches called diverticula in the intestines. These pouches are usually in the lower part of the intestines in the colon.
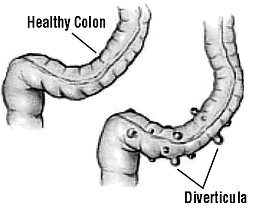
While both diverticulosis and diverticulitis are essentially a condition of “pockets” the one major difference between the two conditions are whether or not the pouches are infected or inflamed. Diverticulitis is where the pockets are infected and can be thought of as a more severe form of diverticulosis. However, the presence of an active infection in diverticulitis makes the treatments of the two conditions very different. (2)
It is important to see a doctor to determine if it is an issue. A doctor will often order a CT scan or a lower GI series, which are x-rays taken after consuming barium sulfate, the drink they give you to examine your digestive system. Due to the presence of bacteria and inflammation in diverticulitis, blood work may also be done. An elevated C-Reactive Protein (C-RP) as well as an elevated White Blood Cell (WBC) count are what your doctor will look for. They may recommend a colonoscopy, however, if the doctor suspects diverticulitis, they will avoid doing a colonoscopy or using a barium enema due to possible side effects. (5)
ICYMI: DIGESTIVE HEALTH PART 7: IBD VS. IBS >> Read Now!
Diverticulosis
While an exact cause for diverticulosis is unknown, there are risk factors. The most well documented risk factor is constipation. In addition, having a low fiber diet, a cause of constipation or a diet heavy in meat consumption are risk factors. Extreme weight loss, advanced age and a genetic predisposition with 40% of people inheriting it are also risk factors. An example of a genetic condition that increases risk is Ehlers Danlos Syndrome (6).
Diverticulosis can cause cramps, gas, bloating, a change in bowel movements and blood in the stool. In fact, diverticular disease is one of the most common causes of lower gastrointestinal bleeding. Unfortunately, diverticular disease is also associated with a higher risk of colon cancer.(3) In addition to these symptoms, diverticulitis can also cause severe pain in the abdomen, nausea, vomiting as well as systemic symptoms such as chills and fever. It can also lead to a loss of appetite, resulting in weight loss.(4) It’s important to have a high fiber diet to avoid constipation, since a low fiber diet and constipation are two of the risk factors.
While some supplement suggestions may be the same for both conditions, the goals are not. For diverticulosis, the goal is to prevent constipation and lower the risk of gut inflammation. Demulcent herbs have been found to be helpful by lowering inflammation in the digestive tract and reducing the incidence of opportunistic infection. Invite’s DGL, Aloe Vera, Slippery Elm and Marshmallow root are some of the herbs that can benefit diverticulosis. (10) Invite’s GI Maintain and Min Acid are also a couple of other options to help lower inflammation.
Diverticulitis
Infection of the pouches or diverticulitis occurs for unknown reasons however there are known additional risks along with the risk factors for diverticulosis. Additional risk factors include obesity, lack of exercise, smoking and use of NSAIDS.
Diet plays a huge role in diverticulitis. Small foods such as nuts and seeds can get “stuck” in the pouches leading to an overgrowth of bacteria. Avoid nuts, seeds and “small foods” that can get stuck in pockets. Eliminating these from the diet decreases a potential risk for complications.(9) Holistically, we know that food allergies/sensitivities can lead to inflammation in the gut. (7) Pathogens can also cause inflammation in the digestive tract.
One of the most dangerous complications is one of the inflamed diverticulum rupturing. This rupture can cause bacteria to spread to the abdomen, causing a very dangerous infection, peritonitis. Side effects can include bowel obstruction, abscess and fistulas, an abnormal connection between organs. (8)
For a flare up of diverticulitis, you want to calm down inflammation and treat the infection. In most cases, treating diverticulitis requires an antibiotic, however there are natural supplements that can work with prescribed medications.
Eat a low fiber diet; it’s important to give the colon a “rest.”(13) Castor oil packs have been found to reduce inflammation and cramps.(14) Colostrum has been found to reduce inflammation in the colon.(15) Invite’s Colostrum and GI Immune, Demulcents, Probiotics, and L-Glutamine are helpful in reducing inflammation present in the colon.
Probiotics are shown in studies to be a promising treatment option for lowering inflammation in the gut and helping both diverticulosis and diverticulitis (11). Invite’s Probiotic Hx, Core Probiotic and Probiotic Weight are supplements that can lower inflammation. L-Glutamine has been found in studies to promote healing in the digestive tract. (12) Invite’s GI Maintain and L-Glutamine promote improved digestive health.
IS PREBIOTIC AND PROBIOTICS THE SAME THING? – INVITE HEALTH PODCAST, EPISODE 563 >> Listen Now!
Sources
- surgicalconsultantsaurora.com/what-we-do/colon-surgery/diverticulosis-and-diverticulitis
- https://www.ucsfhealth.org/education/diverticular-disease-and-diet
- Stefánsson T, Ekbom A, Sparèn P, Påhlman L (August 2004). “Association between sigmoid diverticulitis and left-sided colon cancer: a nested, population-based, case control study”. Scand J Gastroenterol. 39(8): 743–7. doi:1080/00365520410003272. PMID 15513359. S2CID 21100705.
- “Diverticular Disease”. www.niddk.nih.gov. September 2013. Archived from the original on 13 June 2016. Retrieved 12 June 2016.
- Pemberton, John H (16 June 2016). “Colonic diverticulosis and diverticular disease: Epidemiology, risk factors, and pathogenesis”. UpToDate. Retrieved 13 March 2017.
- “Diverticulosis and Diverticulitis”. American College of Gastroenterology.
- Templeton, AW; Strate, LL (August 2013). “Updates in diverticular disease”. Current Gastroenterology Reports. 15 (8): 339. doi:1007/s11894-013-0339-z. PMC 3832741. PMID 24010157.
- “Diverticular Disease”. www.niddk.nih.gov. September 2013. Archived from the original on 13 June 2016. Retrieved 12 June 2016
- Aldoori, WH; Giovannucci, EL; Rimm, EB; Wing, AL; et al. (1994). “A prospective study of diet and the risk of symptomatic diverticular disease in men”. The American Journal of Clinical Nutrition. 60(5): 757–64. doi:1093/ajcn/60.5.757. PMID 7942584.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6065514/
- https://pubmed.ncbi.nlm.nih.gov/27741164/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4369670/
- Spirt, Mitchell (2010). “Complicated Intra-abdominal Infections: A Focus on Appendicitis and Diverticulitis”. Postgraduate Medicine. 122 (1): 39–51. doi:3810/pgm.2010.01.2098. PMID 20107288. S2CID 46716128.
- https://www.healthline.com/health/castor-oil-pack#uses
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8228205/#:~:text=Bovine%20colostrum%20has%20shown%20some,43%2C44%2C45%5D.