Sinus Infections or Sinusitis Part 1
Dr. Claire Arcidiacono, ND
I wanted to talk about sinus infections for several reasons. Obviously, the location of the sinus cavities plays a role in the decision to talk about them during a review of dental health. In addition to location, the symptoms of a sinus infection can mimic other dental concerns. So, I thought a review on sinus infections was a great idea! Let us get into it, shall we?
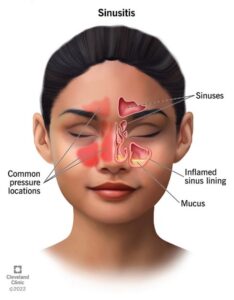
What ARE sinuses? The paranasal sinuses are caves in the bones of our face that produce mucus. These caves are normally filled with air. Paranasal sinuses are arranged in pairs, 1 on the left and one on the right side of our face. I have attached a picture so you can see what this looks like. (1)
As I have said sinuses produce mucus. Now you might not expect me to say this, but mucus does a lot more than just making you blow your nose! Mucus can help fight infections. It also adds moisture and heat to the air you breathe. It is like a natural humidifier! In addition to making mucus the paranasal sinuses do quite a few other things! Since these cavities or caves are hollow, they also reduce the weight of your skull. The sinuses can also serve as “crash zones” that can absorb some of the force during head trauma which can help protect crucial structures such as the brain. Lastly the sinuses can influence how your voice sounds! (1)
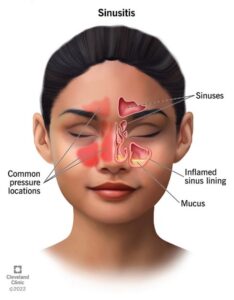
Now that I have reviewed what and where the paranasal sinuses are let us get into the bulk of this blog. That is sinus infections. Now I have been using the term sinus infection but that is really a generic term that is applied to any form of sinusitis. Both acute and chronic sinusitis occur when there is inflammation or swelling in the tissues that line the sinuses. This inflammation can cause them to become blocked and filled with fluid. This is what causes the pressure and pain and other sinusitis symptoms. Please see the attached picture for what this looks like. (2)
As I alluded to there are 2 forms of sinusitis. These are acute sinusitis and chronic sinusitis. Simply put, acute sinusitis is typically caused by viruses and lasts less than 4 weeks. Chronic sinusitis is usually caused by bacteria and lasts more than 12 weeks. Sinusitis lasting between 4 to 12 weeks is usually called subacute sinusitis. If you have acute sinusitis symptoms that come back 4 or more times in 1 year and last less than 14 days (about 2 weeks) each time it is usually called recurrent acute sinusitis. (2)
Sinusitis is usually caused by viruses, bacteria, fungi, and allergens. Something interesting about sinusitis is that while it is not contagious the viruses, bacteria and fungi that lead to sinusitis are all contagious! What are some factors that increase the risk of sinusitis? Having allergies, asthma and nasal polyps all increase the risk of sinusitis. Having a deviated septum is also a risk factor. Smoking or having a weakened immune system can also increase the risk of sinusitis. (2)
What are the symptoms of sinusitis? First, you may feel pressure or pain in your teeth, ears, and face. You may have a stuffy nose, runny nose, and postnasal drip. You may have a cough, headache, fever and feel fatigued. Lastly you may notice bad breath. (2) Now sinusitis can mimic a number of dental issues. In my next blog I will be reviewing how sinusitis is diagnosed. I will also be reviewing how to tell you the difference between a concern with your dental health and with your sinus. Interestingly enough sinusitis can also mimic a cold so I’ll be including a brief description on how to distinguish between the 2 conditions. Lastly, I’ll be reviewing supplements such as Olive Leaf Extract, Green Tea, Black Seed and even my old favorite, NAC!
Sources:
- https://my.clevelandclinic.org/health/body/paranasal-sinuses
- https://my.clevelandclinic.org/health/diseases/17701-sinusitis
- https://www.advancedentdenver.com/blog/sinus-infection-vs-cold-how-to-tell-the-difference/
- https://www.mdpi.com/2079-6382/9/9/526#:~:text=4.,aeruginosa%20infections.
- https://www.webmd.com/diet/health-benefits-olive-leaf-extract
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5884000/#:~:text=The%20results%20of%20investigations%20on,modulator%2C%20antimicrobial%20and%20analgesic%20effects.